Homeopathic Treatment of Asthma
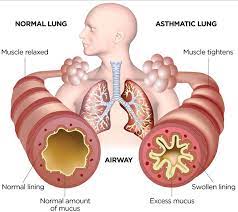
Asthma is the common chronic inflammatory disease of the airways characterized by variable and recurring symptoms, reversible airflow obstruction, and bronchospasm. Asthma affects people of all ages, but it most often starts during childhood. The inside walls of an asthmatic's airways are swollen or inflamed. This swelling or inflammation makes the airways extremely sensitive to irritations and increases susceptibility to an allergic reaction.
Causes of Asthma:
Asthma is caused by a combination of complex and incompletely understood environmental and genetic interactions. These factors influence both its severity and its responsiveness to treatment.
1. Allergies:
Almost all asthma sufferers have allergies. In fact, over 25% of people who have hay fever (allergic rhinitis) also develop asthma. Allergic reactions triggered by antibodies in the blood often lead to the airway inflammation that is associated with asthma.
Common sources of indoor allergens include animal proteins (mostly cat and dog allergens), dust mites, cockroaches, and fungi. It is possible that the push towards energy-efficient homes has increased exposure to these causes of asthma.
2. Tobacco Smoke:
Tobacco smoke has been linked to a higher risk of asthma as well as a higher risk of death due to asthma, wheezing, and respiratory infections. In addition, children of mothers who smoke - and other people exposed to second-hand smoke - have a higher risk of asthma prevalence. Adolescent smoking has also been associated with increases in asthma risk.
3. Environmental Factors:
Allergic reactions and asthma symptoms are often the result of indoor air pollution from mold or noxious fumes from household cleaners and paints. Other indoor environmental factors associated with asthma include nitrogen oxide from gas stoves. In fact, people who cook with gas are more likely to have symptoms such as wheezing, breathlessness, asthma attacks, and hay fever.
Pollution, sulfur dioxide, nitrogen oxide, ozone, cold temperatures, and high humidity have all been shown to trigger asthma in some individuals.
Weather changes have also been known to stimulate asthma attacks. Cold air can lead to airway congestion, bronchoconstriction (airways constriction), secretions, and decreased mucociliary clearance (another type of airway inefficiency). In some populations, humidity causes breathing difficulties as well.
4. Obesity:
Overweight adults - those with a body mass index (BMI) between 25 and 30 - are 38% more likely to have asthma compared to adults who are not overweight. Obese adults - those with a BMI of 30 or greater - have twice the risk of asthma. According to some researchers, the risk may be greater for nonallergic asthma than allergic asthma.
5. Pregnancy:
The way you enter the world seems to impact your susceptibility to asthma. Babies born by Caesarean sections have a 20% increase in asthma prevalence compared to babies born by vaginal birth. It is possible that immune system-modifying infections from bacterial exposure during Cesarean sections are responsible for this difference.
When mothers smoke during pregnancy, their children have lower pulmonary function. This may pose additional asthma risks. Research has also shown that premature birth is a risk factor for developing asthma.
6. Stress:
People who undergo stress have higher asthma rates. Part of this may be explained by increases in asthma-related behaviors such as smoking that are encouraged by stress. However, recent research has suggested that the immune system is modified by stress as well.
7. Genes:
It is possible that some 100 genes are linked to asthma - 25 of which have been associated with separate populations as of 2005.Genes linked to asthma also play roles in managing the immune system and inflammation. There have not, however, been consistent results from genetic studies across populations - so further investigations are required to figure out the complex interactions that cause asthma.
Mom and Dad may be partially to blame for asthma, since three-fifths of all asthma cases are hereditary. Genetics may also be interacting with environmental factors.
8. Airway Hyper-reactivity:
Researchers are not sure why airway hyper-reactivity is another risk factor for asthma, but allergens or cold air may trigger hyper-reactive airways to become inflamed. Some people do not develop asthma from airway hyper-reactivity, but hyper-reactivity still appears to increase the risk of asthma.
9. Atopy:
Atopy - such as eczema (atopic dermatitis), allergic rhinitis (hay fever), allergic conjunctivitis (an eye condition) - is a general class of allergic hypersensitivity that affects different parts of the body that do not come in contact with allergens. Atopy is a risk factor for developing asthma.
Some 40% to 50% of children with atopic dermatitis also develop asthma, and it is probable that children with atopic dermatitis have more severe and persistent asthma as adults.
Signs and Symptoms of Asthma:
Asthma symptoms range from minor to severe and vary from person to person. You may have infrequent asthma attacks, have symptoms only at certain times — such as when exercising — or have symptoms all the time.
Asthma signs and symptoms include:
Signs That Your Asthma is Probably Worsening Includes:
Asthma signs and symptoms those are more frequent and bothersome
For some people, asthma symptoms flare up in certain situations:
Types of Asthma:
1. Child-Onset Asthma:
Asthma that begins during childhood is called child-onset asthma. This type of asthma happens because a child becomes sensitized to common allergens in the environment - most likely due to genetic reasons. The child is atopic - a genetically determined state of hypersensitivity to environmental allergens.
Allergens are any substances that the body will treat as a foreign body, triggering an immune response. These vary widely between individuals and often include animal proteins, fungi, pollen, house-dust mites and some kind of dust. The airway cells are sensitive to particular materials making an asthmatic response more likely if the child is exposed to a certain amount of an allergen.
2. Adult-Onset Asthma:
This term is used when a person develops asthma after reaching 20 years of age. Adult-onset asthma affects women more than men, and it is also much less common than child-onset asthma.
It can also be triggered by some allergic material or an allergy. It is estimated that up to perhaps 50% of adult-onset asthmas are linked to allergies. However, a substantial proportion of adult-onset asthma does not seem to be triggered by exposure to allergen(s); this is called non-allergic adult-onset asthma. This non-allergic type of adult onset asthma is also known as intrinsic asthma. Exposure to a particle or chemical in certain plastics, metals, medications, or wood dust can also be a cause of adult-onset asthma.
3. Exercise-Induced Asthma:
If you cough, wheeze or feel out of breath during or after exercise, you could be suffering from exercise-induced asthma. Obviously, your level of fitness is also a factor - a person who is unfit and runs fast for ten minutes is going to be out of breath. However, if your coughing, wheezing or panting does not make sense, this could be an indication of exercise-induced asthma.
As with other types of asthma, a person with exercise-induced asthma will experience difficulty in getting air in and out of the lungs because of inflammation of the bronchial tubes (airways) and extra mucus.
Some people only experience asthma symptoms during physical exertion. The good news is that with proper treatment, a person who suffers from exercise-induced asthma does not have to limit his/her athletic goals. With proper asthma management, one can exercise as much as desired
Eighty percent of people with other types of asthma may have symptoms during exercise, but many people with exercise-induced asthma never have symptoms while they are not physically exerting themselves.
4. Cough-Induced Asthma:
Cough-induced asthma is one of the most difficult asthmas to diagnose. The doctor has to eliminate other possibilities, such as chronic bronchitis, post nasal drip due to hay fever, or sinus disease. In this case the coughing can occur alone, without other asthma-type symptoms being present. The coughing can happen at any time of day or night. If it happens at night it can disrupt sleep.
5. Occupational Asthma:
This type of asthma is triggered by something in the patient's place of work. Factors such as chemicals, vapors, gases, smoke, dust, fumes, or other particles can trigger asthma. It can also be caused by a virus (flu), molds, animal products, pollen, humidity and temperature. Another trigger may be stress. Occupational asthma tends to occur soon after the patients starts a new job and disappears not long after leaving that job.
6. Nocturnal Asthma:
Nocturnal asthma occurs between midnight and 8 AM. It is triggered by allergens in the home such as dust and pet dander or is caused by sinus conditions. Nocturnal or nighttime asthma may occur without any daytime symptoms recognized by the patient. The patient may have wheezing or short breath when lying down and may not notice these symptoms until awoken by them in the middle of the night - usually between 2 and 4 AM.
Nocturnal asthma may occur only once in a while or frequently during the week. Nighttime symptoms may also be a common problem in those with daytime asthma as well. However, when there are no daytime symptoms to suggest asthma is an underlying cause of the nighttime cough, this type of asthma will be more difficult to recognize - usually delaying proper therapy. The causes of this phenomenon are unknown, although many possibilities are under investigation.
7. Steroid-Resistant Asthma (Severe Asthma):
While the majority of patients respond to regular inhaled glucocorticoid (steroid) therapy, some are steroid resistant. Airway inflammation and immune activation play an important role in chronic asthma. Current guidelines of asthma therapy have therefore focused on the use of anti-inflammatory therapy, particularly inhaled glucocorticoids (GCs). By reducing airway inflammation and immune activation, glucocorticoids are used to treat asthma. However, patients with steroid resistant asthma have higher levels of immune activation in their airways than do patients with steroid sensitive (SS) asthma.
Furthermore, glucocorticoids do not reduce the eosinophilia (high concentration of eosinophil granulocytes in the blood) or T cell activation found in steroid resistant asthmatics. This persistent immune activation is associated with high levels of the immune system molecules IL-2 (interleukin 2), IL-4 and IL-5 in the airways of these patients.
Treatment of Asthma:
Homeopathic Treatment of Asthma:
Asthma is generally a chronic condition, and though there are various homeopathic remedies that can assist in managing an acute episode or the shortness of breath, a “constitutional” homeopathic approach can, in most cases, cures the underlying disposition. The homeopathic “constitutional” approach is one of discovering the individuality of the person suffering from the complaint by taking a holistic portrait; examining not just the symptoms one experiences during an attack, but also understanding the personality and individual temperament. Looking closely at all the changes and variations that occur on the physical, mental and emotional levels in order to determine how a person’s health and well being have become altered. Homeopathy further examines hereditary factors and environmental triggers in order to complete this constitutional portrait. The homeopathic approach stimulates the individual’s own natural forces of recovery by aiming treatment at the cause of the illness instead of prescribing medications based solely on the diagnosis. In conventional medicine they mostly treat the symptoms, but never cure the person, and so attacks are recurrent. In homeopathy we cure the individual thereby eliminating the symptoms.
Quick-Relief Medicines:
All people who have asthma need quick-relief medicines to help relieve asthma symptoms that may flare up. Inhaled short-acting beta2-agonists are the first choice for quick relief.These medicines act quickly to relax tight muscles around your airways when you're having a flareup. This allows the airways to open up so air can flow through them.
Avoid Things That Can Worsen Your Asthma:
Many common things (called asthma triggers) can set off or worsen your asthma symptoms. Once you know what these things are, you can take steps to control many of them. For example, exposure to pollens or air pollution might make your asthma worse. If so, try to limit time outdoors when the levels of these substances in the outdoor air are high. If animal fur triggers your asthma symptoms, keep pets with fur out of your home or bedroom.